Australia case study
As with most developed settings, in Australia people who inject drugs (PWID) are the group at highest risk of infection and transmission; however slow disease progression means that PWID do not necessarily have the heaviest burden of HCV-related liver disease.
Achieving elimination targets will involve responses among both PWID and people with advanced liver disease.
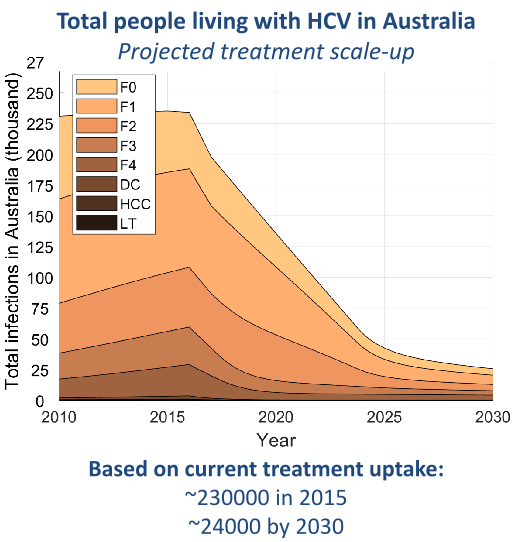
We estimated the treatment scale-up required among PWID and among people with advanced liver disease, as well as the total cost and cost-effectiveness of achieving the World Health Organization incidence and mortality targets in Australia.
We found that
- Approximately 5,700 treatment courses per year are required for patients with advanced liver disease to achieve a 65% reduction in HCV-related mortality in Australia by 2030.
- Approximately 4,700 treatment courses per year are required for HCV-infected people who inject drugs (59/1000 PWID) to achieve an 80% reduction in HCV incidence in Australia by 2030.
- Achieving both targets was estimated to cost AU$4.6 ($4.2-4.9) billion over 15 years; however this was also estimated to be cost-effective, with an incremental cost-effectiveness ratio of AU$25,000 ($11,000-39,000) per quality-adjusted life year gained.
Policy briefs
The Optima HCV model is currently deployed in back-end Python code and can be run by one of our modeling specialists. A front-end version is planned for release in 2019.
To use, contact us at: info@ocds.co
Technical reports
Eliminating Viral Hepatitis – The Investment Case: Report of the WISH Viral Hepatitis Health Forum 2018
Economic evaluation of potential increased hepatitis C treatment uptake in Australia
National Centre in HIV Epidemiology and Clinical Research, University of New South Wales [PDF]
Publications
Modelling the elimination of hepatitis C as a public health threat in Iceland: A goal attainable by 2020
Eliminating hepatitis C virus as a public health threat among HIV-positive men who have sex with men: a multi-modelling approach to understand differences in sexual risk behaviour
Journal of the International AIDS Society , 21(1), e25059 [PDF]
Heterogeneity in hepatitis C treatment prescribing and uptake in Australia: a geospatial analysis of a year of unrestricted treatment access
Hepatitis C virus notification rates in Australia are highest in socioeconomically disadvantaged areas
Eliminating hepatitis C: the importance of frequent testing of people who inject drugs in high prevalence settings
Reaching hepatitis C virus elimination targets requires health system interventions to enhance the care cascade
Treatment scale-up to achieve global hepatitis C virus incidence and mortality elimination targets: a cost-effectiveness model
Limited provision of diagnostic services to Victorians living with hepatitis C antibodies, 2001–2012: a multi‐level modelling analysis
Australian and New Zealand Journal of Public Health , 41(2):193-198
Cost-effectiveness of treating chronic hepatitis C virus with direct-acting antivirals in people who inject drugs in Australia
The potential impact of a hepatitis C vaccine for people who inject drugs: is a vaccine needed in the age of direct-acting antivirals?
The role of a hepatitis C virus vaccine: modelling the benefits alongside direct-acting antiviral treatments


 © Optima Consortium for Decision Science, Burnet Institute, Melbourne, 2025
© Optima Consortium for Decision Science, Burnet Institute, Melbourne, 2025